Our Blog
My Pet’s Tooth is Discolored. What Does It Mean?
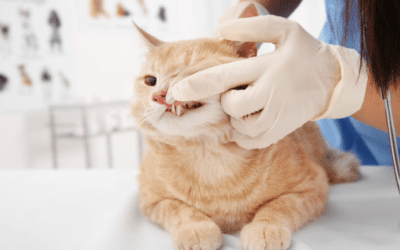
Regular visual inspection of your pet’s mouth and teeth is an important part of your pet’s home dental care routine. If you notice that one or more of their teeth is an abnormal color, it is essential to discuss this change with your primary care...
Tooth Extractions: When and Why Are They Needed?
Maintaining good oral hygiene is just as important for our pets as it is for us. However, even with regular cleaning, a pet's tooth may need to be extracted for various reasons. Extraction, or surgical removal of a tooth, can be performed by a...
Pet Dental Health Month: Resolve to Start a Good At-Home Dental Care Routine
February is Pet Dental Health Month -- the perfect time to start a fresh new dental care routine for your pet! Starting an at-home dental care routine is an important part of responsible pet ownership. Just like humans, pets require regular dental...
What is Tooth Resorption?
Tooth resorption, also previously called feline odontoclastic resorptive lesions (FORLs) or simply resorptive lesions (RLs), was previously thought to only exist in cats, but is a common dental condition in which the tooth structure begins to break...
Gift Guide: Picking the Best Toys for Your Pet’s Teeth
The holiday season is upon us and if you’re like many pet owners, that means giving gifts to your pets, too! We all want our pets to join in on the holiday festivities, but we also want them to be safe while doing so. Believe it or not, there are...
Why is Anesthesia Necessary for Dental Procedures?
One of the main concerns pet owners have about dental procedures is their pets undergoing anesthesia. While anesthesia does carry some inherent risks, it is a necessary part of the dental procedure. Going to the dentist is a scary endeavor for many...
Oral Masses (Tumors) in Cats and Dogs
Finding an oral mass (or tumor) in your pet’s mouth can be alarming. You may wonder what this means for your pet and what happens next. At Veterinary Dentistry Specialists, our team of board-certified veterinary dentists and board-certified...
Frequently Asked Questions About Advanced Veterinary Dental Care
All pets need veterinary dental care at some point during their lives. Depending on the level of dental care needed, your primary care veterinarian may recommend referral to a board-certified veterinary dentist™ (also referred to as a specialist)...
Would You Know if Your Pet Was Suffering From Oral Pain?
Did you know dental problems in pets are very common? Approximately 80% of dogs and 70% of cats over 3 years of age have some form of oral disease. The pain associated with dental disease can range from discomfort to agonizing for your pet, and...
Feline Chronic Gingivostomatitis
Feline Chronic Gingivostomatitis (FCGS) is a painful and potentially debilitating condition of cats, characterized by widespread inflammation in the oral cavity. It is typically seen in cats ranging from 3-10 years of age but has been identified in...
Dentigerous Cysts
Dentigerous cysts are a relatively common dental condition in dogs. This condition can also occur in cats, but it is much less common in this species. While any breed of dog can develop a dentigerous cyst, small breeds appear to be predisposed to...